The number of people in England waiting to start hospital treatment has returned to record levels, though times for the longest waits have improved, figures show.
Ambulance and A&E performance has held steady, despite the NHS continuing to face pressures from bed shortages, winter viruses and strike action.
The proportion of cancer patients receiving their first treatment within two months of an urgent GP referral has dropped to a record low, however.

An estimated 7.21 million people were waiting to start routine hospital treatment at the end of January, up from 7.20 million in December, according to new figures from NHS England.
It is the joint highest total since records began in August 2007. This was previously reached in October 2022.
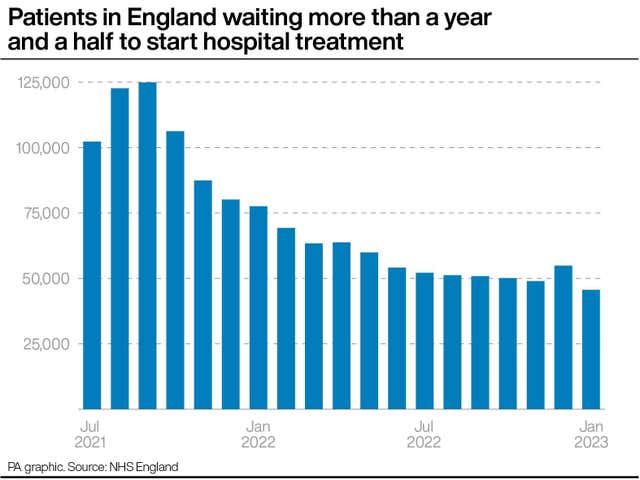
The number waiting more than a year and a half to start treatment has dropped month-on-month by 17% from 54,882 to 45,631, in a sign that progress is being made on clearing the backlog of longest waits.
The Government and NHS England have set the ambition of eliminating all waits of more than 18 months by April 2023, excluding exceptionally complex cases or patients who choose to wait longer.
Waits of more than 52 weeks are down from 406,035 in December to 379,245 in January, with a target for eliminating them completely by March 2025.
The latest NHS performance figures for England also show that:
– The average response time in February for ambulances dealing with the most urgent incidents, defined as calls from people with life-threatening illnesses or injuries, was eight minutes and 30 seconds, unchanged from January but above the target standard response time of seven minutes.
– Ambulances took an average of 32 minutes and 20 seconds last month to respond to emergency calls such as heart attacks, strokes and sepsis, up very slightly from 32 minutes and six seconds in January, while the target is 18 minutes.
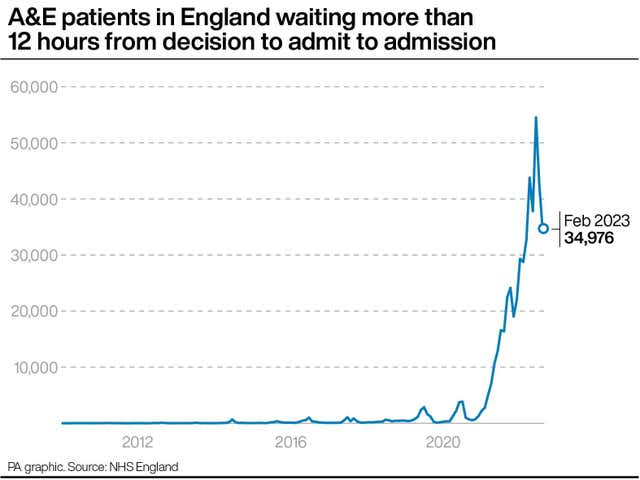
– The number of people waiting more than 12 hours in A&E departments from a decision to admit to actually being admitted stood at 34,976 in February, down 18% from 42,735 in January and down 36% from a record 54,532 in December 2022.
– The number waiting at least four hours from the decision to admit to admission has fallen from 142,139 in January to 126,948 in February, a drop of 11%.
Performance against cancer targets is mixed.
Some 228,197 urgent cancer referrals were made by GPs in England in January, up both month-on-month (by 7% compared with December 2022) and year-on-year (by 12% compared with January 2022).
But just 54.4% of the 15,401 cancer patients who had their first treatment in January after an urgent GP referral waited less than two months, down from 61.8% the previous month and the lowest proportion since records began in 2009.
The target for this measure is 85%.
Meanwhile, 67.0% of patients urgently referred for suspected cancer were diagnosed or had cancer ruled out within 28 days in January, down from 70.7% the previous month.
Dr Ian Walker, executive director of policy at Cancer Research UK, said the figures highlight a “devastating situation for patients and their loved ones who are now facing the worst waits on record to start their treatment”.
“Every month, thousands of cancer patients don’t start their treatment within the target timeframe and a key reason is that cancer services are chronically understaffed,” he added.
“If the Government is serious about being ‘laser-focused’ on cancer, it must publish a fully costed NHS workforce plan for England. Without this it is going to be extremely difficult to ensure more people survive cancer for longer.”
Professor Stephen Powis, NHS national medical director for England, said there had been “no let-up” of pressures, with staff facing “significant levels of respiratory illness in hospital, which came at the same time as disruption from industrial action”.
He continued: “Despite this, staff continued to deliver for patients, bringing down elective waits, treating more cancer patients and delivering more diagnostic tests for people than ever before.
“Not only that, but ambulance response times in February for the most serious callouts sustained improvements seen in January. This is a huge achievement. We are extremely grateful for the enormous efforts from staff, who we know are tired, after an extremely challenging few months.
“The NHS will not stop in its efforts to bring down 18-month waits for elective care and bring down the cancer backlog, but it is inevitable that if the upcoming junior doctors strikes happen they will have a significant impact on cancer care and routine operations that were scheduled to happen – as ever, we will do all we can to limit the impact to patients.”
Junior doctors in England are due to begin a 72-hour strike on March 13 in an ongoing dispute about pay.
Industrial action by ambulance workers that had been scheduled for this week was suspended after the Government agreed to discuss salary levels for this year.
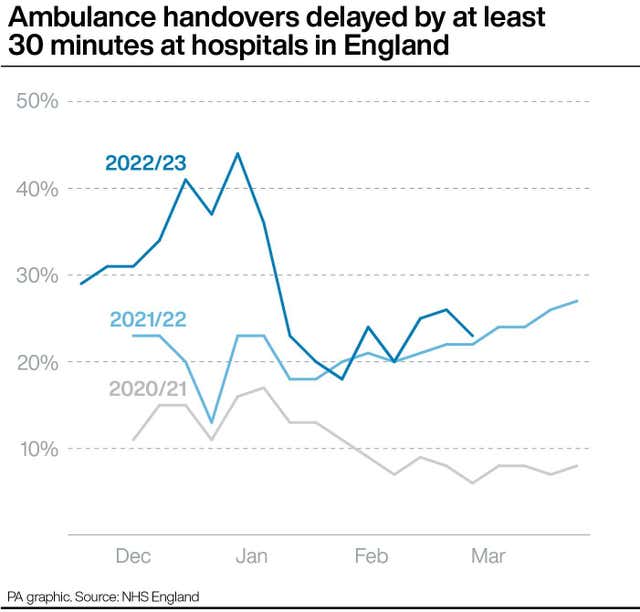
Separate figures published on Thursday show ambulance handover delays outside hospitals in England improved slightly last week, though levels are still higher than at this point last year.
Some 23% of ambulance patients were kept waiting at least half an hour before being transferred to A&E departments, down from 26% the previous week and the first fall since early February.
The figure stood at 22% in the equivalent week in 2022.
The proportion of ambulance patients waiting for more than an hour was 9%, down week-on-week from 11%.
Meanwhile, an average of 13,272 hospital beds per day were occupied by people ready to be discharged, 13% higher than the 11,745 waiting a year ago.
Both sets of data reflect the ongoing challenge faced by hospitals in finding room for new arrivals, with handover delays linked to the shortage of space caused by people who no longer need to be in beds.
Overall, 42% of medically fit patients in England were discharged last week, but the rate varies considerably between regions, from 32% in the North West to 53% in eastern England.
Sir Julian Hartley, chief executive at NHS Providers, the membership organisation for NHS trusts in England, said the “very high” level of ambulance handover delays and delayed discharges “reflects the fundamental mismatch between demand and capacity across all systems”.
“This slows down patient flow across the health and care services, including in mental health and community care,” he added.
“Recovery is extremely fragile and trust leaders are concerned that ongoing pressure from industrial action and staff shortages could block progress.
“The long-term workforce plan, which needs to be fully funded, should help alleviate some of this stress. We hope the chancellor announces it in the Budget next week.”




Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules here